Description
Includes your full personal report and plan from Jo, with a Zoom consultation to run through the diagnosis and prognosis.
What is the Complete Hormones™ test?
Complete Hormones™ is Genova’s most comprehensive urinary hormone profile, and is designed to assist with the clinical management of hormone-related symptoms in both male and females. This profile assesses parent hormones and their metabolites as well as key metabolic pathways, provides insight into the contribution that sex hormones may have in patients presenting with hormone-related complaints, and helps assess disease risk associated with elevated estrogen metabolites.
Urine measures the most metabolites, providing more insight into associated disease risk.
The Complete Hormones profile evaluates:
- Progesterone (via pregnanediol)
- Glucocorticoids, including cortisol
- Androgens, including DHEA and testosterone, and their metabolites
- Estrogens (E1 Estrone, E2 Estradiol, E3 Estriol) and metabolites, including hydroxylated and methoxylated estrogens
- Methylation capacity
- 5α-reductase activity
- Anabolic/Catabolic Balance
The unique report configuration provides for easy interpretation and clinically actionable results:
- The Steroidogenic Pathway-At-A-Glance page allows the clinician to see patient results along the metabolic cascade, allowing a quick assessment of potential areas of concern in hormone production and metabolism.
- The Interpretation-At-A-Glance page summarizes results through color-coded graphic representations of overall hormonal balance and metabolism, highlighting key ratios for easier test interpretation and clinical application.
When should the Complete Hormones test be considered?
The Complete Hormones test is designed to assist in the management of hormone-related symptoms in both males and females.
The Complete Hormones test is ideal for establishing a baseline assessment of parent hormones and their metabolites ahead of clinical intervention with hormone therapy (HT) as well as subsequent monitoring if needed in both female and male patients.
The Complete Hormones test provides insight into the impact that shifting hormone levels may play in men (andropause or male menopause) and women (peri/menopause). Symptoms include the following:
- Weight gain
- Anxiety
- Fatigue
- Muscle mass loss
- Muscle weakness
- Low libido and sexual performance issues
- Hair loss
- Sleep disturbances
- Brain fog
- Mood instability
- Hot flashes
- Vaginal dryness
In addition to supporting patient management around hormone-dependent symptoms, the profile provides valuable insight into disease risk for hormone-associated cancers (breast, prostate) and osteoporosis.
What advantage does Complete Hormones profile offer compared to other hormone tests?
The conventional clinical approach to hormone-related symptoms (such as those experienced by patients in the perimenopause/menopause transition) does not routinely include utilization of comprehensive urine hormone testing. When testing is performed, basic parent-hormone blood testing is generally the test of choice, since serum testing is well represented in the literature. However, urinary assays provide several advantages over blood assays for patients with hormone-related symptoms.
- Steroid hormones naturally fluctuate over the course of a day and measurement of hormones in urine collected over several hours provides a stable average of hormone levels that overcomes the âsnapshotâ limitation inherent in serum testing.
- Emerging research reinforces the potential relationship of disease risk with individual hormone metabolites, particularly downstream estrogen metabolites â especially those of the 4-hydroxylation pathway. Given the close interrelationships of steroid hormones, a comprehensive assessment comprising these metabolites is recommended, at least for an initial evaluation. Complete Hormones provides measurement of these metabolites with a convenient patient-friendly collection for people with normal renal function who are not on diuretic medications.
- In addition to the measurement of multiple steroid hormones and enzymatic pathways, this profile also measures indicators for the effects of stress on an individual. The Anabolic/Catabolic Balance refers to the balance between âgrowth and healingâ (anabolic) and âwear and tearâ (catabolic) in the body. Both anabolic and catabolic metabolism are essential to health. For example, a healthy body requires sufficient time and androgens to rebuild/repair cells (anabolic), but also sufficient corticosteroids to respond to stressors and to discharge cellular debris/toxins (catabolic).
- The Interpretation-At-A-Glance page summarizes results through color-coded graphic representations of overall hormonal balance and metabolism, highlighting key ratios for easier test interpretation and clinical application.
What can clinicians and patients expect from Complete Hormones testing?
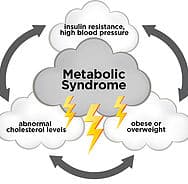
Imbalanced or insufficient hormone production affects a wide range of body functions, producing symptoms that negatively affect the quality of life.
Imbalanced or insufficient hormone production affects a wide range of body functions, producing symptoms that negatively affect the quality of life and, with some metabolic pathways, may increase risk for hormone-related diseases. A structured diagnostic hormone panel — such as Complete Hormones — to evaluate underlying hormonal imbalances provides clinical utility by supporting insight into development of personalized treatments. Identification and targeted treatment of underlying hormonal imbalances with customized HT and/or nutritional interventions improves symptoms and quality of life — and may reduce disease risk.
Parent Hormones
- Personalized HT based on clinical symptomology and urine hormone assessment
A/C Balance
- Supportive therapeutics for modulating a high or low A/C Balance include stress management, adequate sleep, reducing stimulants such as caffeine, reducing high glycemic load foods, and adrenal nutritional and botanical support.
5α-Reductase Activity
- Therapeutic strategies for 5α-reductase inhibition include pharmaceutical intervention with 5α-reductase inhibitors (such as Finasteride) or botanical inhibitors (such as saw palmetto).
Unfavorable estrogen metabolite profile
- In patients with a low 2-hydroxylation result, metabolism may be shifted toward this pathway by dietary interventions rich in cruciferous vegetables; exercise that increases lean body mass and decreases BMI; and supplementation with indole-3-carbinol (I3C) or diindolylmethane (DIM), as well as omega-3 fatty acids, and B vitamins.
Compromised methylation
- Numerous factors support methylation including SAMe; the amino acid, methionine; magnesium; B vitamins including folate; trimethylglycine (TMG); glutathione; and stress management strategies that reduce catecholamine production.
- Studies demonstrate that when DNA is incubated with quinones in the presence of an antioxidant, the formation of the DNA adducts is reduced. Support of antioxidant activity appears to be a reasonable proactive step for reducing risk of hormone-related disease. Several natural compounds have exhibited the ability to minimize DNA adduct formation including resveratrol, N-acetylcysteine (NAC), lipoic acid, and melatonin. Cruciferous and allium vegetables also demonstrate the ability to induce glutathione S-transferases.








Reviews
There are no reviews yet.